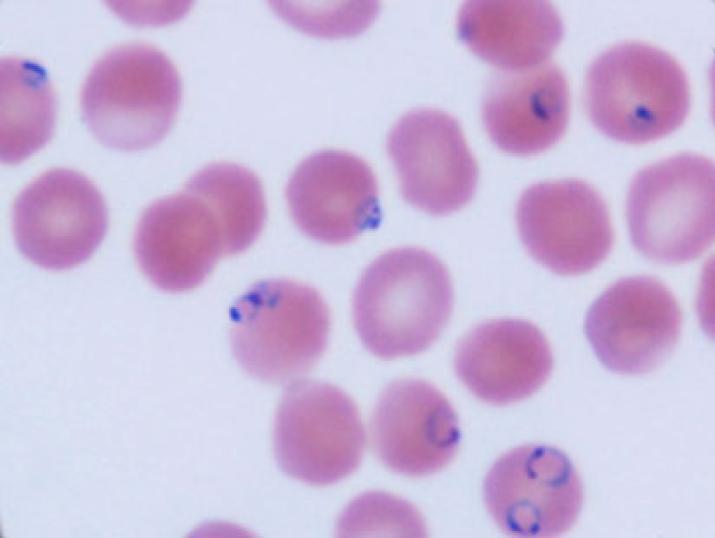
Photograph of malaria parasites in red blood cells in the blood of one of the study's participants
Published March 24, 2015 under Research News
When patients are suffering from the most severe form of malaria, known as cerebral malaria, infected red blood cells are trapped within the microscopic vessels of the brain. This impedes critical oxygen delivery, resulting in coma and often leading to death.
Previous studies by an international team of malaria researchers had shown that this condition is also marked by lower production of nitric oxide in the cells lining these micro-vessels. Reversing this deficiency could help prevent malaria-infected red cells from sticking to blood vessel walls and avoid this dire condition.
A follow-up study by these researchers in Tanzania, Indonesia, Australia and the U.S. has shown one reason for poor nitric oxide production. A critical co-factor for an enzyme that produces nitric oxide must be “charged” with potential energy.
This co-factor is called tetrahydrobiopterin (abbreviated BH4). It exists in both energy-rich (“charged”) and energy-drained “discharged” forms. In normal cells, the BH4 “battery” is always poised in the “charged” state.
Measuring these molecules in children and adults with severe malaria, the researchers found that while the body has plenty of the co-factor, its form was discharged and therefore unable to supply the energy needed for nitric oxide synthesis.
Why has the “battery” run down? The answer requires more research, but the investigators speculate that oxygen radicals produced during the inflammation associated with malaria may be draining energy from BH4.
Their results were published in two companion papers in the current issue of PLoS Pathogens.
The researchers are now trying to determine if there is a way to provide new energy to BH4. Existing therapies for treating vascular disease may hold some promise, the researchers said.
Field research in Dar es Salaam, Tanzania was led by Professor Esther Mwaikambo of the Hubert Kairuki Memorial University, and in Timika, Papua Indonesia by Dr. Nicholas M. Anstey and Dr. Tsin Yeo of the Menzies Institute for Medical Research, Darwin, Australia. The U.S. investigators were affiliate Duke Global Health Institute faculty member Dr. J. Brice Weinberg and Dr. Matthew Rubach of Duke University School of Medicine and Durham Veterans Affairs Medical Center and Dr. Donald L. Granger, University of Utah School of Medicine and Salt Lake City Veteran Affairs Medical Center. The research was supported by grants from the U.S. National Institutes of Health and the Veterans Affairs Research Service (Dr. Granger and Dr. Weinberg); and by the Australian National Health and Medical Research Council (Dr. Anstey).
Citations:
“Impaired Systemic Tetrahydrobiopterin Bioavailability and Increased Oxidized Biopterins in Pediatric Falciparum Malaria: Association with Disease Severity,” Rubach MP, Mukemba J, Florence S, Lopansri BK, Hyland K, Volkheimer AD, Yeo TW, Anstey NM, Weinberg JB, Mwaikambo ED, Granger DL. PLoS Pathogens, March 12, 2015. DOI:10.1371/journal.ppat.1004655
“Impaired Systemic Tetrahydrobiopterin Bioavailability and Increased Dihydrobiopterin in Adult Falciparum Malaria: Association with Disease Severity, Impaired Microvascular Function and Increased Endothelial Activation,” Yeo TW, Lampah DA, Kenangalem E, Tjitra E, Price RN, Weinberg JB, Hyland K, Granger DL, Anstey NM. (2015) PLoS Pathogens, March 12, 2015. DOI:10.1371/journal.ppat.1004667


