Multisystemic Comorbidity-IBD Relationships in the SPARC IBD Cohort

Project member(s):
-
Haley Cionfolo
Faculty mentor:
-
Jane Onken
Community partners:
-
The Crohn's and Colitis Foundation of America, IBD Plexus Division
Tara Fehlmann
Sirimon O'Chaeron
- Feedback? Contact the team
Multisystemic Comorbidity-IBD Relationships in the SPARC IBD Cohort
Project overview
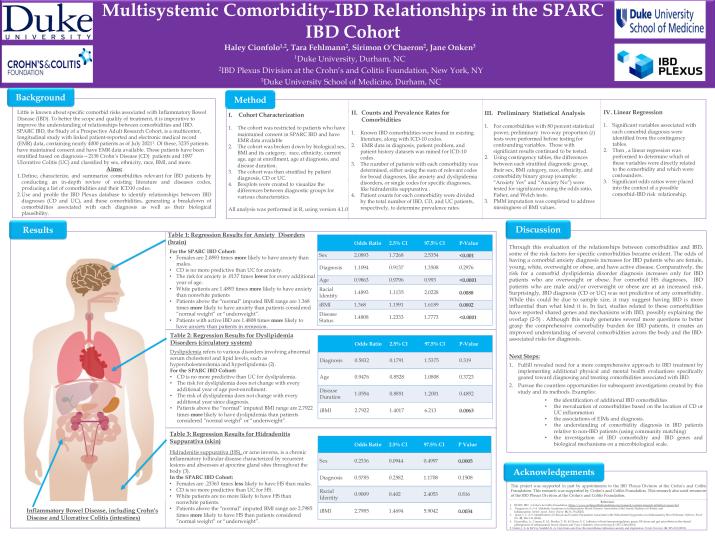
Little is known about specific comorbid risks associated with Inflammatory Bowel Disease (IBD), nor do any existing study designs investigate different IBD comorbidities separate organ systems within the same study. To better the scope and quality of treatment, it is imperative to improve the understanding of the relationships between comorbidities and IBD. SPARC IBD, the Study of a Prospective Adult Research Cohort, is a multicenter, longitudinal study with linked patient-reported and electronic medical record (EMR) data, containing nearly 4000 patients as of July 2021. Of these, 3235 patients have maintained consent and have EMR data available. These patients have been stratified based on diagnosis—2138 Crohn’s Disease (CD) patients and 1097 Ulcerative Colitis (UC) and classified by sex, ethnicity, race, BMI, and more.
The aims of this study were to (1) characterize comorbidities relevant for IBD patients by conducting an in-depth review of existing literature and diseases codes and to (2) use and profile the IBD Plexus database to identify relationships between IBD diagnoses (CD and UC), and these comorbidities. Through this evaluation of the relationships between comorbidities and IBD, some of the risk factors for specific comorbidities became evident. The odds of having a comorbid anxiety diagnosis increases for IBD patients who are female, young, white, overweight or obese, and have active disease. Comparatively, the risk for a comorbid dyslipidemia disorder diagnosis increases only for IBD patients who are overweight or obese. For comorbid HS diagnoses, IBD patients who are male and/or overweight or obese are at an increased risk. Surprisingly, IBD diagnosis (CD or UC) was not predictive of any comorbidity. While this could be due to sample size, it may suggest having IBD is more influential than what kind it is. In fact, studies related to these comorbidities have reported shared genes and mechanisms with IBD, possibly explaining the overlap. Although this study generates several more questions to better grasp the comprehensive comorbidity burden for IBD patients, it creates an improved understanding of several comorbidities across the body and the IBD- associated risks for diagnosis.
Last updated on June 26, 2023